Cerebral edema, or brain swelling, is a dangerous condition that should be treated as early as possible in order to prevent severe complications. This article will address the effective ways of treating and managing cerebral edema, encompassing information regarding medical, surgical, and lifestyle treatments aimed at enhancing symptoms and patient outcomes.
Overview of Cerebral Edema
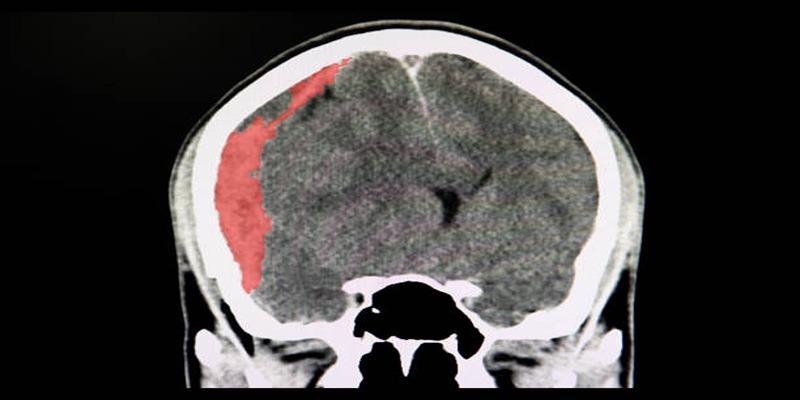
We will begin with the general characteristics of cerebral edema. Cerebral edema is a term that refers to a pathological accumulation of fluid within brain tissues, thereby raising pressure in the skull. The condition may result from traumatic injuries to the brain, stroke, infection, or specific medical ailments like liver or kidney failure.
Higher pressure can lead to compression and injury of sensitive brain structures, producing an array of symptoms from headache, nausea, and vomiting to confusion and loss of consciousness. In some cases, cerebral edema can lead to permanent brain damage or even death if not timely treated.
Types of Cerebral Edema
Cerebral edema can be divided into some different types according to the mechanisms of swelling. These types are important in deciding the treatment and management strategies. The primary types of cerebral edema are given below:
1. Vasogenic Edema
This type of edema is the one where there is a loss of integrity of blood-brain barrier, and fluid leaks out from vessels into brain extracellular space. The etiology is commonly tumors, abscesses, or trauma. Vasogenic edema affects the white matter and in the majority of instances is secondary to pathologies that expand vascular permeability. Detection early in the course by imaging techniques such as MRI is essential to treat it effectively with medicines such as corticosteroids or surgical intervention in selected instances.
2. Cytotoxic Edema
Cytotoxic edema results from injury to brain cells, i.e., neurons, glial cells, or endothelial cells, typically because of ischemia or hypoxia. Unlike vasogenic edema, in cytotoxic edema, intracellular accumulation of fluid takes place because of the failure of sodium-potassium pumps. It results from stroke, cardiac arrest, or toxin ingestion.
Cytotoxic edema is found in gray and white matter and quickly becomes severe if not treated. Treatment is typically directed at correcting the underlying cause, such as re-establishing brain oxygenation or using medicine to stabilize cellular processes.
3. Osmotic Edema
Osmotic edema follows from an imbalance of osmotic pressure between the blood and brain, which permits the entry of water into cells in the brain. It may result from hyponatremia, overhydration, or too rapid correction of hypernatremia.
The subsequent swelling affects brain function and may result in serious neurological complications. Effective management typically involves cautious correction of electrolyte imbalance and monitoring to avoid additional osmotic shifts, allowing the brain to stabilize gradually.
4. Interstitial Edema
Interstitial edema is most commonly caused by hydrocephalus or cerebrospinal fluid (CSF) blockage, leading to an intracranial accumulation of the fluid in the periphery of the brain. The accumulated fluid compresses the neighboring structures of the brain and leads them to become swollen. Interstitial edema primarily occurs in white matter of the periventricular area and is primarily observed in meningitis or hemorrhage of the brain.
Treatment may involve the insertion of a shunt to drain excess CSF or medications to decrease production of fluid, alleviating pressure from brain tissues. Early detection and management are crucial for this type of edema.
Treatment Strategies
Successful management of edema depends on a holistic approach that is specific to the cause and the severity of the condition. Some of the most important treatment strategies employed in practice are described below.
Medical Interventions
These interventions aim to reduce swelling, alleviate symptoms, and address the root cause of edema to prevent further complications.
Use of Corticosteroids
Corticosteroids are commonly employed to reduce inflammation and cerebral edema, particularly in cases involving brain tumors or certain inflammatory conditions like meningitis. These medications work by stabilizing the blood-brain barrier and decreasing vascular permeability, which leads to a reduction in fluid accumulation.
Dexamethasone is one of the most frequently used corticosteroids in such scenarios. However, the use of corticosteroids must be carefully monitored due to potential side effects, including immunosuppression, hyperglycemia, and gastrointestinal complications.
Osmotic Therapy
Osmotic therapy, using agents such as mannitol or hypertonic saline, is another primary intervention for managing cerebral edema. These substances create an osmotic gradient that helps draw water out of swollen brain tissues and into the bloodstream, thereby reducing intracranial pressure (ICP). Mannitol is administered through intravenous infusion and acts quickly, making it a preferred option in emergency situations.
Hypertonic saline solutions are also effective in improving cerebral perfusion and reducing brain swelling. Dosing and patient response must be closely monitored to avoid complications like electrolyte imbalances or renal impairment.
Surgical Interventions

If medical management does not adequately control intracranial pressure, surgical interventions may become necessary to address the underlying cause and alleviate pressure effectively.
Decompressive Craniectomy
Decompressive craniectomy is a surgical procedure in which a portion of the skull is temporarily removed to allow the swollen brain to expand without being constrained by the cranial vault. This intervention is often considered for patients suffering from severe traumatic brain injury, stroke, or other life-threatening conditions associated with significant intracranial pressure.
The removed skull segment is usually preserved for later reattachment once the swelling subsides. Although highly effective in reducing ICP, this procedure carries risks such as infection, bleeding, and long-term neurological deficits.
Ventricular Drainage
Ventricular drainage, also known as an external ventricular drain (EVD), involves the insertion of a catheter into the brain's ventricles to remove excess cerebrospinal fluid (CSF). This method effectively alleviates pressure within the cranial cavity and is particularly beneficial in cases of hydrocephalus or intracranial hemorrhage.
The procedure requires precision and is typically performed in a controlled surgical setting to minimize the risk of infection or injury to surrounding brain tissues.
Supportive Care
This approach is often complemented by additional interventions to ensure optimal patient recovery and overall management of the condition.
Monitoring Intracranial Pressure
Continuous monitoring of intracranial pressure is a critical component of managing cerebral edema. ICP monitoring devices, such as intraparenchymal sensors or EVD systems, provide real-time data that guide physicians in making timely and effective treatment decisions. Maintaining ICP within a safe range is essential for preventing further brain damage and optimizing patient outcomes.
Oxygen and Ventilation Support
Ensuring adequate oxygenation and ventilation is vital for patients with cerebral edema. Hypoxia can exacerbate brain swelling and worsen outcomes, making oxygen therapy and mechanical ventilation indispensable in severe cases. Adjustments in ventilation settings may also help to manage CO2 levels, as hypercapnia can lead to vasodilation and increased intracranial pressure. Close collaboration between neurology and critical care teams is essential to balance oxygen delivery and minimize additional complications.
Conclusion
Effective management of cerebral edema requires a multifaceted approach, prioritizing timely interventions and continuous monitoring. By addressing underlying causes, optimizing ventilation, and ensuring multidisciplinary coordination, healthcare providers can improve patient outcomes and mitigate complications. Advances in research and clinical practices will further enhance our ability to treat this complex and critical condition effectively.












